Combining the capabilities of UnitedHealthcare and Optum for greater health plan value
Using its strengths as a payer, a care delivery organization and a tech and data company enable UnitedHealth Group to stay at the forefront of health care innovation.
Greater health plan value with UnitedHealthcare and Optum
When clients work with UnitedHealthcare, they tap into the power of UnitedHealth Group. The enterprise — entrusted to help provide health benefits and services to 250M+ members worldwide — includes Optum, a technology and data-enabled health care services company.
UnitedHealth Group has been a leader in the charge to transform health care for more than a decade, investing upwards of $5B annually in innovation, research and development and technology.1 Its businesses, UnitedHealthcare and Optum, are both laser-focused on bringing solutions to market that help people live healthier lives and help make the health system work better for everyone. And each uses unique capabilities to carry out this mission.
UnitedHealthcare brings decades of experience in developing health plans and benefits designed to meet the needs of employers and their employees. Optum then brings its clinical expertise, technology and data from serving as a pharmacy benefit manager (PBM) and health services administrator. The capabilities of both companies help power better health outcomes, lower costs and simpler experiences.
Enterprise-enabled collaboration
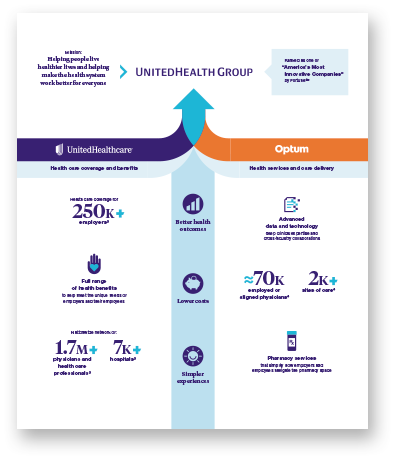
UnitedHealth Group brings together the health care coverage and benefits of UnitedHealthcare and the health services and care delivery of Optum.
UnitedHealth Group was ranked as one of “America’s Most Innovative Companies” by Fortune2
UnitedHealthcare provides health care coverage for more than 250K employers3
Optum has 70K employed or aligned physicians4
Redefining the standard of quality care
To fuel meaningful innovation, a shared philosophy is critical.
“When we talk about aligning with another business, it doesn’t just mean a contractual relationship,” says Stephanie Alberti, vice president of product for UnitedHealthcare Employer & Individual. “It’s a meeting of the minds where philosophically we agree about the best way to care for members.”
For instance, both data and experience show:
- How important the primary care provider (PCP) is to the health of a patient
- That not all providers are alike when it comes to delivering quality care
As a leading health solution and care delivery organization, Optum is continually focused on expanding its network of providers and developing health solutions that aim to meet people where they are at every stage of their care journey.
This includes establishing strategic relationships with different providers and provider groups across the country who are delivering a level of quality care that is in line with UnitedHealthcare and Optum standards. Then, UnitedHealthcare works to design health plans that prioritize or incentivize access to those high-value providers.
Reimagined health plans such as Surest™ build on this shared philosophy of quality care. Offering access to the broad, national UnitedHealthcare network, the Surest health plan uses a unique pricing model to help members find cost-efficient treatments and quality care from high-value providers. Through clinical advocacy and Optum clinical services, Surest identifies and engages members to assess needs and clinical opportunities.
Another example is a new health plan addition being developed by UnitedHealthcare and Garner Health. Using data science and advanced analytics, Garner Health assesses and recommends high-value providers and then incentivizes members for following the recommendation by contributing the cost of seeing that provider into their health reimbursement account (HRA).
Evolving strategies to meet changing health needs
UnitedHealthcare and Optum also work together to ensure members have access to a continuum of care throughout their health journey.
Improving care accessibility requires innovating and developing solutions that allow members to get care when and where they need it, including virtually. At UnitedHealthcare, virtual visits are available to eligible members for a variety of needs powered by Optum technology, including 24/7 urgent care, primary care, behavioral health care and specialty care. More accessible care can also look like getting care at home, at retail clinics or even at the workplace.
With a desire to help create a healthier community and work environment, one large employer in Kansas, built an on-site clinic for its employees with the support of UnitedHealthcare. The employee health center also includes a workout facility and a pharmacy, making it more convenient for employees and their families to stay on top of their health.
Convenience and accessibility are also the driving forces behind home delivery of prescriptions.5 With Optum® Home Delivery, safety and convenience aren’t sacrificed for innovations in the prescription delivery space. UnitedHealthcare members can rest easy, knowing that each prescription undergoes a rigorous safety and quality process, even as most orders are quickly processed within 3–5 days.
Optum is at the forefront of improving the cost of pharmacy benefits and prescription drugs, while also providing strategic advice that may lead to better health outcomes and lower costs.
External collaborations
In addition to collaborating internally, UnitedHealthcare and Optum understand that collaborating with external entities and supporting health startups matters:
Optum Ventures: A venture capital firm that invests in entrepreneurs who are working to bring innovative solutions to everything from virtual behavioral health for families to metabolic weight loss.
UnitedHealthcare Accelerator: A program that brings together 10 world-class health tech start-ups each fall for a collaborative program that surrounds them with leading health care experts invested in their succes.
“We unlock the full potential to support our customers and members with simpler health care experiences by collaborating and integrating the power of UnitedHealthcare, Optum and external entities.”
– Kelley Nolan-Maccione, Chief Product Officer, UnitedHealthcare Employer & Individual
Developing data-driven, insight-led, tech-forward solutions
UnitedHealthcare and Optum have access to data around claims, labs, gaps in care and more. This data enables UnitedHealthcare and Optum to bring forward rich point-of-care solutions, which can help promote better health outcomes and lower costs to better serve their members and customers.
For instance, Point of Care Assist® embeds real-time patient information — including clinical, pharmacy, labs, prior authorization and cost transparency — into existing electronic medical records (EMRs) to make it easier for providers to understand what patients need at the point of care. PreCheck MyScript® is another example. Integrated directly with an EMR, it allows providers to get real-time prescription coverage details for their UnitedHealthcare-covered patients.
Moving forward, data insights like these may accelerate the process of getting more personalized, evidence-based care recommendations for any number of conditions.
“By collaborating with Optum, UnitedHealthcare is able to develop a more integrated and coordinated health care system that uses technology and personal support to help encourage whole-person health, which may help prevent and detect disease before it starts,” says Dr. Rhonda Randall, chief medical officer at UnitedHealthcare Employer & Individual.