Expanding behavioral health network strategies to provide greater access to care
A shortage of providers challenges health plans to find new approaches to help meet the growing demand.

Demand for mental health services is straining capacity, according to a recent survey.1 In fact, 6 in 10 providers reported that they no longer have openings for new patients.1 This isn’t surprising given that the U.S. is experiencing a growing psychiatrist shortage.2 And diversity in networks is lacking, as about 8 in 10 psychologists are white.3
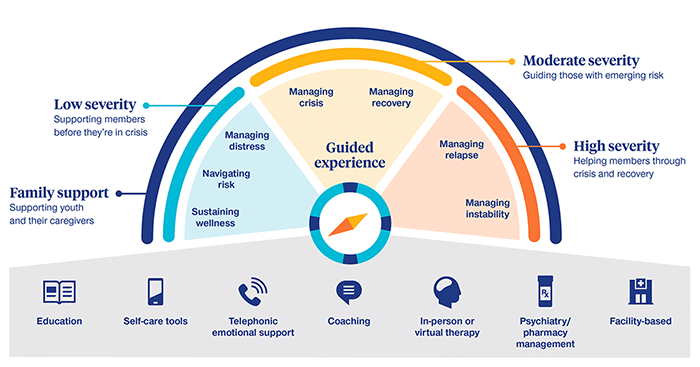
To help address these challenges, UnitedHealthcare efforts focus on more than growing the network of providers. It also includes reducing barriers to accessing care and increasing engagement across a comprehensive continuum of care from self-help apps to inpatient treatment. This approach is designed to address different levels of behavioral health conditions more effectively by helping to guide members to the level of care they may need—and adjusting the level of care as needed.
With more than 315,000 providers and 136,000 state-licensed virtual care providers,4 strategies to help provide greater access include:
Planning for future behavioral health needs
The pandemic created momentum around virtual care and it’s not slowing down. In fact, 40% of recently surveyed adults used virtual care in 2022, and nearly 4 out of 5 said virtual health made it easier for them to seek out care when they needed it.5
At UnitedHealthcare, more than half of behavioral health visits in 2020 were virtual for employees with UnitedHealthcare coverage.6
“Most of my patients prefer virtual. It’s eliminated commuting and wait times in the office. At first, I had reservations about switching to virtual care, especially with new patients, but it hasn’t made a difference working with them,” says Martin H. Rosenzweig, chief medical officer of Optum Behavioral Health, which supports UnitedHealthcare behavioral health benefits.
These new virtual offerings are designed to help meet the needs of individuals and improve access to care.7 Offering virtual care options may also reduce the stigma around seeking mental health support. This is especially true among the older population, as the stigma tends to prevent older adults from seeking care versus younger adults who are more accepting of mental health care.7
Offering specialty behavioral health care
Incorporating virtual care and providing specialty services may help manage specific behavioral health conditions more effectively.
Specialized solutions include support for those with eating disorders, substance use disorders, pharmacy and medication management services for employees with behavioral health conditions and medication-assisted treatment with group counseling for opioid addiction.
UnitedHealthcare has more than 48,000 substance use disorder providers,4 and nearly 9,600 medication-assisted treatment locations, with 96% of members living within 20 miles of a provider.8 For instance, Genoa Healthcare, one of the largest providers of pharmacy, outpatient telepsychiatry and medication management services, has a network that includes 6,400 prescribers, including 3,500 telepsychiatrists across nearly all 50 states.9
Providing preventive mental health care to help avoid crises
Offering a continuum of care may make it easier for employees to take proactive measures to help maintain their mental health and overall well-being similar to physical health. This approach may help prevent a mental health condition from progressing in severity.
To help reduce barriers of entry, engagement and medical and behavioral coordination, UnitedHealthcare has worked to develop and launch virtual behavioral therapy and coaching, which proactively outreaches and connects members to a licensed behavioral specialist to help address their condition.
“Historically, a member’s first step into behavioral health has been a therapist or psychiatrist. What we found is that not all members need that level of care,” Grassmuck says. “We’ve brought forth more options like a self-help app that can help get at contributing factors of depression and stress, and behavioral health coaching that can help mitigate triggers.”
Increasing network diversity for minorities, children and teens
During the pandemic, mental health conditions impacted many populations, but were the most profound among women, teens and racial minority groups.7 Employers can help address this with targeted campaigns to highlight available resources and services, such as virtual care that may help reduce stigma.
“We found mental health disparities in these populations worsened during the course of the pandemic,” says Dr. Rhonda Randall, executive vice president and chief medical officer for UnitedHealthcare Employer & Individual.
Stigma may also be more prevalent in some minority groups, and evidence shows that some minority groups do not seek mental health support as often as their white counterparts. Among adults with any mental illness, 48% of white adults received mental health services compared to 31% Black and Hispanic adults and 22% of Asian adults.10
To support network diversification by raising cultural competency and promoting network diversity, UnitedHealthcare has worked to promote:
- Strategic recruitment of specialty providers, such as medication-assisted treatment providers
- Cultural competency training
- Adding ethnicity, gender and language as provider search criteria
- Scholarships for child psychiatrists and providers from diverse backgrounds
“Data shows more licensed professionals in all 50 states, but some areas of the country lack certain types of providers,” Randall says. “We’re always looking for ways to expand and diversify our network while supporting providers who are feeling the strain of increased demand.”
Those efforts along with increasing the virtual care network, specialty care in areas such as substance use and encouraging preventive mental health care to avoid crises play a role in creating greater behavioral health access for employees and their families.