Leveraging data analytics to help increase employee engagement for better outcomes
Combining data and targeted communications helps employers tailor their benefits strategy to help improve the member experience and lower costs.
Employee populations are diverse and complex—geography, demographics, type of work, interests and values all play a role in defining unique individuals. And considering that about half of Americans have employer-based health care coverage,1 there’s no shortage of health-related data available for analysis. What employers do with that data, though, can help define their health benefits strategy.
UnitedHealthcare uses advanced analytics to process multiple sources of data—ranging from claims to physical and behavioral health data—to help create a more personalized member experience and drive engagement. By identifying unique populations and sub-populations, employers may provide these employees with more tailored support to navigate the health system.
For instance, about 3%–5% of those with complex care needs reported 5 times the number of claims than those without advanced needs.2 And about 1% of those with complex care continued needs drove more than 30% of the total cost for care.2 This illustrates why treating a complex care population the same as the general population leaves opportunity on the table for cost efficiency and overall member engagement.
“There’s more than enough data in health care. What we do is filter it all down, craft the right message and in order for employers to act upon it—it’s part science, part art and one of the key competencies we have in the marketplace,” says Craig Kurtzweil, chief analytics officer for UnitedHealthcare Employer & Individual.
The ability to find actionable solutions from data allows employers to:
3 key takeaways about health care data analysis
- Sophisticated data analytics allows employers to understand what’s behind high utilization, engagement and cost at an individual level within their employee population.
- Employers can turn those insights into high-touch, personalized member outreach.
- Employees may be more likely to access high-quality and low-cost care, manage their chronic conditions, and avoid costly services after they’ve received targeted communications.
Pinpointing precise opportunities to help employees who need more care
When analyzing sub-populations, combining UnitedHealthcare’s proprietary analytics capabilities with an employee’s background information provides an opportunity to tailor more relevant communications. This can include an employee’s age, gender or geography, and employment information such as division, job type or salary.
While a large national employer’s population may appear healthy overall when viewing the data in aggregate, Kurtzweil explains that a closer look at one of its locations may reveal a more targeted opportunity for engagement based on condition prevalence in a sub-population, such as a group of employees with type 2 diabetes struggling to effectively manage the condition.
By leveraging the employer’s health care data, UnitedHealthcare discovered that, although there were quality, cost-efficient designated UnitedHealth Premium® providers in the area, the employees weren’t utilizing them. The nature of their work made it difficult for the employees to make appointments during regular business hours, Kurtzweil explains.
Through on-site events with providers that engaged both the employees and leadership—a key component to any effective employee engagement effort— employees began complying with measures such as medication adherence to help manage their condition. This approach helped the employer address an employee pain point and find the right solution for their employees.
“Our sophisticated approach allows us to deliver the right message to the right members at the right time to help produce the desired result. We’re customizing what we do to meet members where they’re at,” Kurtzweil says.
Targeting members with timely messages
Advanced data analytics helps employers understand what drives high utilization, engagement and cost at an individual level within their population and turn those insights into personalized member outreach.
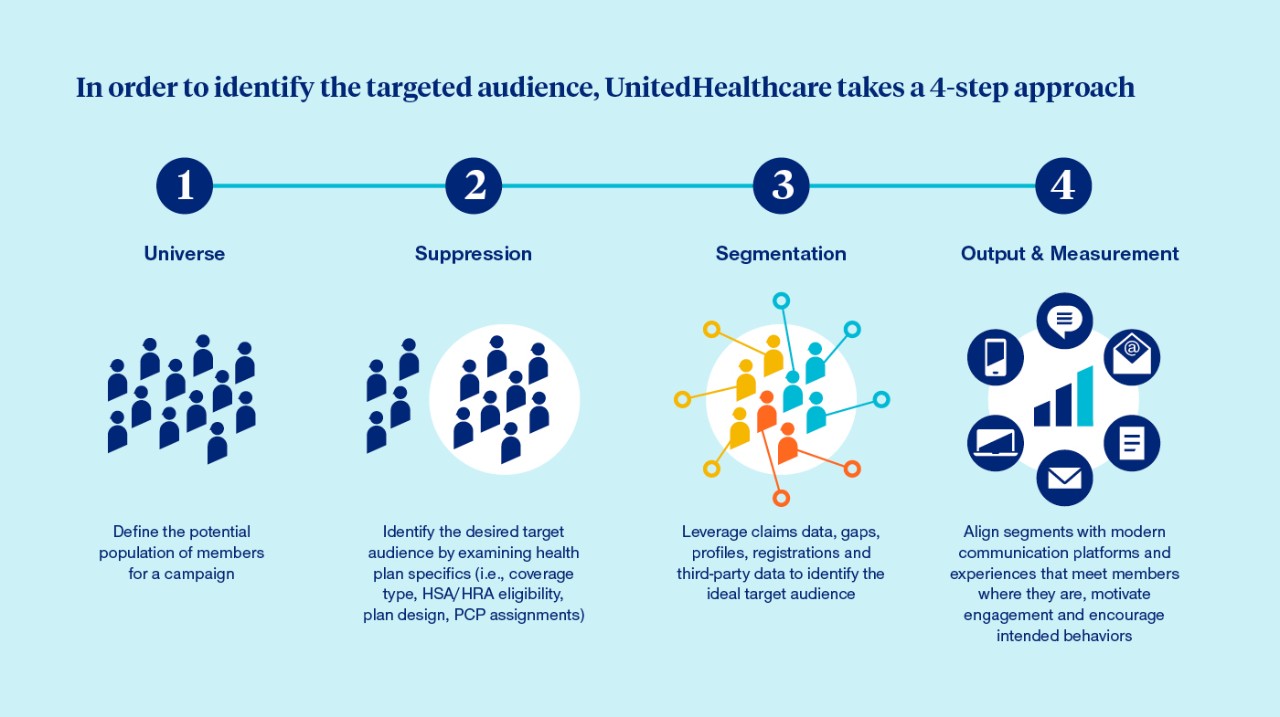
Employers can implement targeted interventions by working with their benefits team and through collaborating with UnitedHealthcare Engagement Solutions, a health engagement and communications consultancy that specializes in developing and deploying population-specific engagement strategies, communications plans and custom health activation materials for large employers.
“We use the power of our data and the strength of our organization to really understand where our members are in their health care journeys and put that knowledge into action,” says Cheryl Mau, vice president of Engagement Solutions at UnitedHealthcare.
Knowing 73% of consumers expect companies to understand their unique needs and expectations,3 Engagement Solutions takes a modern and multi-channel approach to meet members where they are with tailored and original content campaigns that motivate optimal health care decisions. More informed, confident and proactive employees—and their families— are more likely to access quality and lower-cost care, manage their chronic conditions and avoid costly services after they’ve received targeted communications.
After the campaigns conclude, employers receive performance measurement reports that include the actions their employees took and the impact targeted engagement had on cost savings. The performance reports also help to inform future communications. In 2022, targeted campaign strategies developed by Engagement Solutions helped deliver $35M in savings for their clients.4
The impact of segmentation targeting was brought to life for 10 employers struggling with high-cost musculoskeletal claims. Employees from each employer received education around treatment options and assistance in connecting to care providers who turn to pain management and surgical alternatives before surgery. The result was $3.5M in cost savings over a 2-year period.5
“Unlike traditional marketing, we can be far more specific about what benefits members have and how to access them,” Mau says. “We’re always looking for creative ways to understand where a member is on their journey and where we can help.”
In order to identify the targeted audience, UnitedHealthcare takes a 4-step approach:
Understanding the effect of social determinants of health on employee wellness
Research shows that medical care accounts for about 20%6 of modifiable contributing factors for positive health outcomes and well-being, while social determinants of health such as education and employment have an even greater impact.
While claims data is valuable, it’s important for employers to also consider dynamics such as poverty and health disparities to understand the why behind health care decisions individuals make. It helps to determine if there are any benefit gaps to address.7
“There is only so much that can be gleaned from claims data, and there are headwinds and tailwinds that make a significant impact in what the claims look like at the end of the day,” Kurtzweil says.
For example, when an employer discovered high, unnecessary utilization of the ER, the UnitedHealthcare data analytics team discovered that the plant location was in a high-crime area.
This caused many employees to not engage with primary care physicians on health conditions that eventually led to the need to use the ER. To address the challenge, the employer added an on-site nurse to tackle less complex health issues and implemented a strategy to promote telehealth and digital capabilities, Kurtzweil says.
UnitedHealthcare works with employers to address how social disparities and racial inequities impact employee health, and refer members into appropriate programs in their communities. When employers address employee needs beyond physical health, they may achieve a more productive workforce and lower health care costs.
“We believe our expertise working with employers, community organizations and other collaborators will help make systemic changes in the health care system,” Kurtzweil says.