Transparency in Coverage Rule
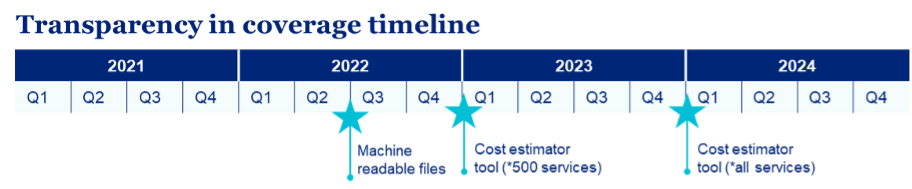
In 2020, the Federal Government finalized “Transparency in Coverage” Rule, which requires health insurers and group health plans, including self-funded clients, to provide cost-sharing data to consumers via:
- Machine-readable files: Machine-readable files must be published on a publicly available site based on the enforcement date of July 1, 2022, for plan years beginning on or after Jan. 1, 2022. These files provide pricing data for covered items and services based on in-network negotiated payment rates and historical out-of-network allowed amounts. A third machine-readable file for prescription* drug rates and historical costs has been delayed pending further guidance. Information in these files must be updated and published monthly. Publicly available MRF
- Consumer price transparency tool: This online tool for members will include personalized, real-time, cost-share estimates for covered services and items, including pharmacy. Paper versions must be available upon request. For plan years beginning on or after Jan 1, 2023, the online tool must provide cost-share estimates for 500 shoppable services. For plan years beginning on or after Jan. 1, 2024, the online tool must provide cost-share estimates for all covered services.
UnitedHealth Group has long supported actionable price and quality transparency for consumers and currently offers transparency tools to a significant portion of our business. Compliance with the laws and regulations applicable to our business is a fundamental commitment of UnitedHealth Group, and we intend to comply with the requirements of the new rules.
Transparency in Coverage Machine Readable Files
Machine-readable files 7/1/22 launch. Refer to FAQ section on Day 1 for Questions
The machine-readable files must be available on an internet website free of charge. The user is not required to establish a user account, password, or other credentials and does not require the user to submit any personal identifying information such as a name, email address, or telephone number.
· Files have requirements regarding font size, accessibility, and security settings.
· Files may be posted on a third party site.
· Files may not be a PDF or Excel. UnitedHealthcare files will be published in JSON.
In-network machine-readable files include negotiated rates for all covered items and services at the plan level, for all medical codes, for contracted rates and by provider.
Out-of-network machine-readable files include allowed amounts for covered items, services based on billed charges and allowed amounts including historical amounts. Files are not required if there are fewer than 20 claims for a service for a provider.
UnitedHealthcare creates and publishes files where we have access to the data on behalf of customers unless otherwise directed by the client. UnitedHealthcare’s publicly available website is transparency-in-coverage.uhc.com (accessible July 1, 2022). Customers may put a link to the UnitedHealthcare site on their website.
Customers who have opted out of their files being published to the UnitedHealthcare public website must retrieve files from a dedicated website -- https://private-transparency-in-coverage.uhc.com/(accessible July 1, 2022). The customers must publish the files monthly to their own publicly available website. Customers are able to retrieve their machine-readable files by July 1, 2022, and monthly thereafter.
Transparency in Coverage Consumer Price Transparency Tool
Starting with plan years beginning on or after January 1, 2023, insurers and plans must make an online price transparency tool available for 500 shoppable items, services and drugs identified in the final rule. All covered items, services, and drugs are required to be included in the consumer price transparency tool for plan years that begin on or after January 1, 2024.
Consumers will be able to get real-time estimates of their cost-sharing liability for health care items and services from different providers. The tool requirements allow the members to understand how costs for covered health care items and services are determined by their plan.
The tool must make available personalized out-of-pocket cost information as well as the underlying negotiated rates and allowed amounts for all covered health care items and services including prescription drugs. The information must be available through an internet-based self-service tool. A paper form of the estimate is available via contact with customer service
Resources for Transparency in Coverage