How a well-managed health plan may benefit Millennials — and their employers
Millennials, which make up the greatest share of the workforce, are beginning to use the health system more, but employers can implement tactics that may help improve outcomes and reduce costs.
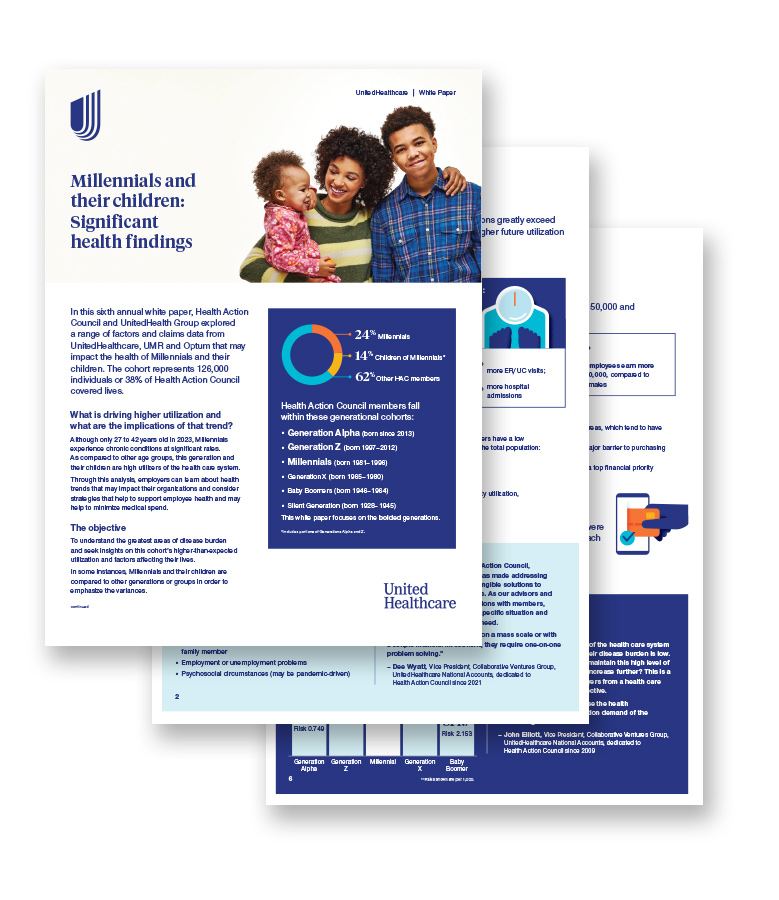
Millennial employees and their children are experiencing higher rates of chronic health conditions than older generations and are utilizing medical resources in significantly different ways.1
That’s according to a recent white paper, commissioned by Health Action Council (HAC) and UnitedHealth Group, the parent company of UnitedHealthcare.
Why this matters to employers: Millennials are the dominant generation covered by employer-sponsored health plans, and they’re growing: The Millennial workforce will increase by nearly 4.5M by 2029, which constitutes the largest gain for a single age group.2 With Millennials’ rising numbers and their high utilization of the health care system, employers should consider how to best accommodate their Millennial-dominant workforce.
Millennial employees and their children are experiencing higher rates of chronic health conditions than older generations and are utilizing medical resources in significantly different ways.1
That’s according to a recent white paper, commissioned by Health Action Council (HAC) and UnitedHealth Group, the parent company of UnitedHealthcare.
Why this matters to employers: Millennials are the dominant generation covered by employer-sponsored health plans, and they’re growing: The Millennial workforce will increase by nearly 4.5M by 2029, which constitutes the largest gain for a single age group.2 With Millennials’ rising numbers and their high utilization of the health care system, employers should consider how to best accommodate their Millennial-dominant workforce.
Millennial trends in utilization and treatment
When compared to other generations, Millennials exceed utilization and treatment for costly medical conditions:1
- Diabetes – 106% more hospital admissions
- Hypertension – 55% more emergency room (ER) and urgent care (UC) visits
- Obesity – 31% more ER/UC visits and 29% more hospital admissions
- Back disorders – 22% higher ER/UC visits and 46% higher admissions
- Osteoarthritis – 36% higher ER/UC visits
In addition to exceeding utilization for chronic conditions like diabetes and obesity, Millennials are also utilizing behavioral health services at disproportionate rates. In fact, Millennials and their children account for 41% of neurodevelopmental disorder claims.1
Pregnancy, however, was the top clinical cost driver, accounting for 21% of employer per member per month (PMPM) spend. The average employer paid between $17,000 and $27,000 per pregnancy.1 Complicating factors, such as fertility treatments, high-risk pregnancies, multiple births, extended hospital stays and C-Section deliveries, contributed to inflated costs.1
With high utilization and an increasing prevalence of costly medical conditions, employers may wonder how to best care for their Millennial employees while also managing their costs.
A well-managed plan can help
A well-managed health plan may help increase health literacy, reduce health risks and decrease expensive hospitalizations and emergency visits.
Align benefits to utilization rates
Analyzing employee data by generation, as well as by market or gender, among other criteria, can offer valuable insights into the root causes and unique needs of an employer’s workforce. It can also help inform employers about which health plan designs and networks to offer their workforces. For Millennials who choose plan designs with the smallest impact to their paychecks, a tiered network that offers quality care, cost savings and a broad range of choices coupled with opportunities for boosting health plan literacy may be a good combination.
Implement healthy lifestyle programs
Disease prevention and lifestyle modification programs may help ward off costly chronic conditions, which can also affect on-the-job productivity. Employers can help foster healthy living by providing access to in-person fitness facilities and virtual fitness courses. They may also want to encourage the formation of employee-led health and well-being committees based on shared health and well-being interests or goals.
Educate employees on their health
Primary care providers (PCP) can be integral in helping employees navigate the complicated health care system, but many Millennials don’t have a PCP.1 Employers may want to fill in the knowledge gap. With UnitedHealthcare, educating employees on their health could mean offering timely communications themselves with the Employee Engagement Planner® (EEP). Or it might mean enlisting the support of Field Account Managers (FAMs) or brokers to educate employees on everything from the importance of immunizations and preventive care, such as blood pressure, diabetes and cholesterol screenings.
Support employee mental health
With employee behavioral health utilization rising, employers may want to do what they can to both provide access to integrated behavioral health and medical benefits while also limiting workplace stress. Offering opportunities for employees to help identify and solve on-the-job challenges or taking steps to create a work culture that fosters a sense of social belonging can go a long way to supporting employees.
Offer financial planning help and resources
Millennials, mostly in their mid-to-late 20s, carry greater medical debt than older Americans and incur it more often.3 High levels of financial stress can have an effect on both an employee’s mental and physical health. Anxiety, depression, high blood pressure and a compromised immune system can all be the fallout. Employers may help mitigate those outcomes with financial planning services, student loan repayment benefits, education funding strategies and debt management education that can all work in concert to help build staff knowledge and confidence over time.
