5 ways to help employees in Tennessee find the behavioral health care they need
As some employees in Tennessee struggle for access amidst dramatic changes in the behavioral health care system, here’s what employers can do to help guide employees to quality, affordable care.
Behavioral health issues are on the rise.1 In fact, more than 1 in 4 employees have quit a job because of their mental health, while 1 in 5 say their company doesn’t do enough for their mental health, according to a recent survey.2
“The whole world at a minimum has experienced more stress, which has contributed to the increase in diagnosis for anxiety and depression, substance use and alcoholism, and prescriptions for behavioral health treatment. Suicide rates have gone up in all populations,” says Dr. Rhonda Randall, executive vice president and chief medical officer for UnitedHealthcare Employer & Individual.
Why this matters to employers in Tennessee: Recent findings identify Tennessee as 1 of the top 10 worst states for behavioral health care based on a variety of measures, including the prevalence of unmet behavioral health needs, the lack of nearby behavioral health facilities and those who are uninsured and living with a mental illness.3 So, employers that operate in Tennessee or that employ people living in Tennessee may want to consider strategies that help support their employees’ mental health needs.
Given these trends, the stakes couldn’t be higher for employers. When employees and their family members experience emotional distress, which may manifest as sleep problems, aches and pains, and low motivation, it may affect their quality of life and may lead to tardiness and missed days at work, lower work quality, safety-related mishaps and the need for medical care.
UnitedHealthcare’s behavioral health strategy is designed to help employees find care across a comprehensive continuum of care. And it includes the promotion of general well-being and treatment of conditions, such as substance use.
Employers can help employees find the behavioral health care by:
- Promoting virtual care to help improve access to provider
- Building a benefits strategy that includes a full continuum of care
- Offering a guided experience to support employees and their families
- Trying to reduce stigma especially for at-risk populations
- Reinforcing the connection between physical and behavioral health
The importance of quality behavioral care
Promote virtual care as a proven strategy for improving access to providers
Evidence suggests that the COVID-19 pandemic has accelerated the demand for behavioral health care for years to come, and consumers will continue to have a growing need for faster, easier access to mental health support.4 With the U.S. only fulfilling 27% of its total need for mental health professionals, there will be a shortage of at least 245,000 behavioral health providers by 2025.5
“Data shows more licensed professionals in all 50 states, but some areas of the country lack certain types of providers,” Randall says. “One of our solutions that helps to address these disparities is virtual care. It enables mental health professionals the ability to obtain licensure across state lines.”
Innovative and effective digital tools, including virtual care solutions, are designed to help meet the needs of individuals and improve access to care. The pandemic created momentum around virtual care, including virtual therapy, that is not slowing down.
- 56% of behavioral health visits in 2020 were virtual for UnitedHealthcare members6
- 77% of employers plan to offer mental health support, including through virtual care and digital tools7
- More than half of U.S. adults are likely to use virtual tools for behavioral health needs8
- Providers are seeing 50–175 times more patients virtually than they have before8
“Most of my patients prefer virtual. It’s eliminated commuting and wait times in the office. At first, I had reservations about switching to virtual care, especially with new patients, but it hasn’t made a difference working with them,” says Dr. Martin H. Rosenzweig, chief medical officer of Optum Behavioral Health, which supports UnitedHealthcare’s behavioral health benefits.
Offering virtual care options may also reduce the stigma surrounding seeking mental health support. Stigma tends to prevent older adults from seeking care versus younger adults who are generally more accepting of mental health care. Stigma is also more prevalent in some minority groups.7
UnitedHealthcare’s behavioral health network alone includes 315,000 providers and 136,000 virtual providers.9
Build a benefits strategy that provides access to a full continuum of solutions
UnitedHealthcare provides comprehensive support across a continuum of care designed to cover a range of employee needs from digital self-help tools to facility-based treatment. This model helps employees take preventive measures to maintain their mental health and overall well-being similar to physical health. As with other aspects of well-being, the focus of employers’ efforts should move from reactive to preventive.10
Because employees don’t always know they have behavioral health benefits and services, UnitedHealthcare helps create awareness by promoting it during open enrollment, onboarding and throughout the year. This helps to encourage the idea of getting care sooner, often before an employee knows they need help.
Solutions such as online education, self-help apps or coaching help equip employees with the tools they need to manage stress, burnout and anxiety. If an employee enters in the system through a crisis, they may access therapy or psychiatric treatment that may require medication or facility-based treatment.
“Our goal is to normalize mental well-being and think of it as common as maintaining physical health similar to seeking a wellness visit each year,” says Trevor Porath, vice president of behavioral health solutions for UnitedHealthcare Employer & Individual. “We want to make every single touch point with a member an opportunity to advance mental well-being.”
To build a more robust continuum of care, UnitedHealthcare has evaluated many vendors, bringing in solutions that fill in care gaps, including AbleTo® and Self Care to support identification, proactive outreach and virtual care delivery, and Equip and Genoa Healthcare for data and medication management and specialty behavioral health.
UnitedHealthcare behavioral health care continuum
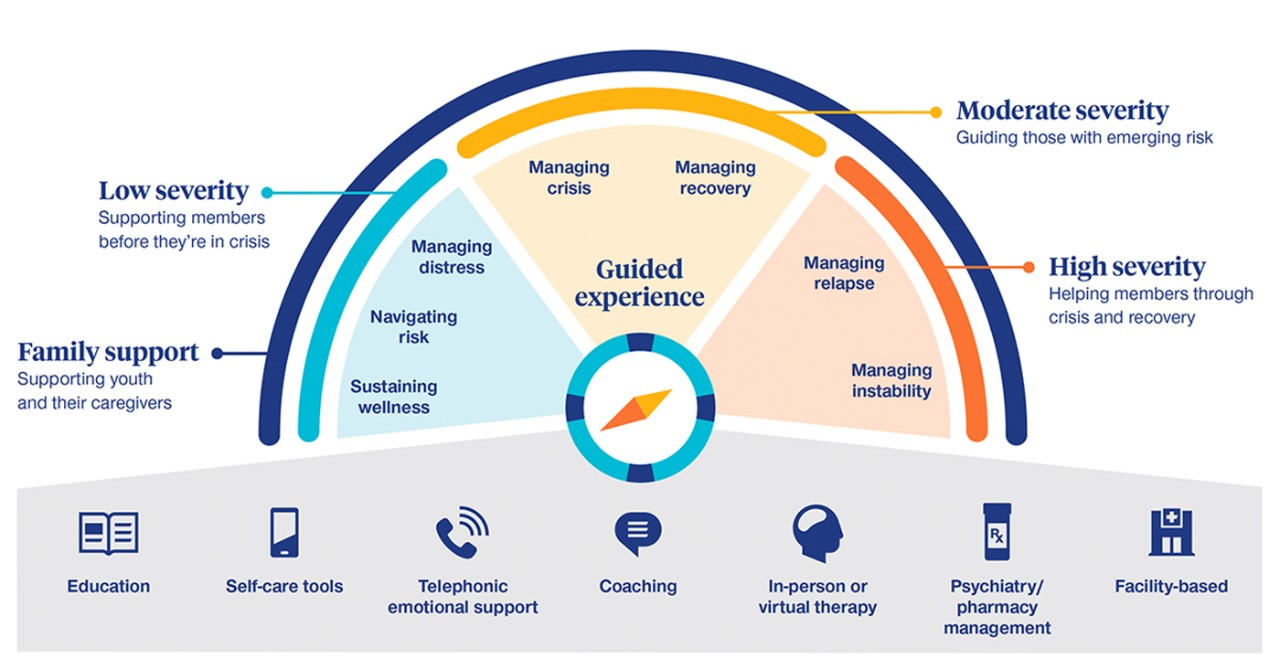
Offer a guided member experience designed to support employees and their families
Low behavioral health literacy remains a challenge for consumers. They don’t often recognize brand names for tools and resources or have a clear understanding of what terms like coaching mean when related to their mental health care.11
A member-guided experience, whether it starts through an Employee Assistance Program (EAP), primary care physician (PCP), care advocate or digitally, helps lead to an evidence-based recommendation on the continuum of care.
“Advocates are trained to listen for signs of distress when speaking to members,” Randall says. “They also help guide members through the complexities of behavioral health including understanding provider types such as social workers, counselors and psychiatrists.”
Predictive tools also help identify members who may need behavioral health support. Pulling from data such as diagnostic codes and utilization patterns, members are segmented based on their conditions—both the level of severity and stability—as well as their ability to engage. This information is used to support advocates or make program suggestions when an employee signs in to myuhc.com®.
For those without a behavioral health diagnosis or utilization of services, a prediction can be made on their level of risk based on social determinants of health data and prevalence of chronic disease—2 of the most critical factors that put employees at risk of developing or having an untreated behavioral condition.
Try to reduce stigma among employees, especially in at-risk populations
During the pandemic, mental health has impacted all populations but has been the most profound among women, teens and racial minority groups.7 Employers can help address this with targeted campaigns to highlight available resources and services such as virtual care that helps reduce stigma.
“It’s so important to be compassionate with mental health due to stigma. Many employees are still afraid and ask if seeking these services will be reported back to their employer,” says Heather Nelson, an advocate trained to provide medical and behavioral health support. “I reassure them an employer only receives general data on program use, which lets them know what their employees need.”
In addition, minority groups may not seek mental health support as often as their white counterparts. Among adults with moderate or severe anxiety and/or depression, 64% of white adults received mental health services compared to 47% of Black adults and 60% of Hispanic adults.12
Diverse populations are more likely to utilize support from a provider of the same race since it makes them feel more comfortable and less judged. Currently, more than 80% of members in the American Psychological Association are white and less than 5% of members are African American.13
To support network diversification by raising cultural competency and promoting network diversity, UnitedHealthcare’s plan has included:
- Strategic recruitment of specialty providers such as medication-assisted treatment providers
- Cultural competency training
- Provider ethnicity, gender and language as provider search criteria
- Scholarships for child psychiatrists and providers from diverse backgrounds
Reducing stigma at the workplace
Employers may help reduce stigma by avoiding language that could potentially hurt or inadvertently discourage someone from seeking mental health treatment. This includes:
| Don't use | Use |
| Words that may reinforce stereotypes and minimize the importance of understanding mental health conditions, such as crazy, head case, lunatic | Specific and sympathetic language |
| A mental health condition to define the person | “Someone who lives with a mental health condition” or “someone who is affected by a mental health condition” |
| The disease to describe the person | A person-first approach such as “a person living with schizophrenia” or “someone diagnosed with schizophrenia” |
Reinforce the connection between physical and behavioral health for better care coordination
UnitedHealthcare claims data show members with comorbid conditions have claims costs that are, on average, twice the claims for members with medical conditions alone.14
In an average group plan population:14
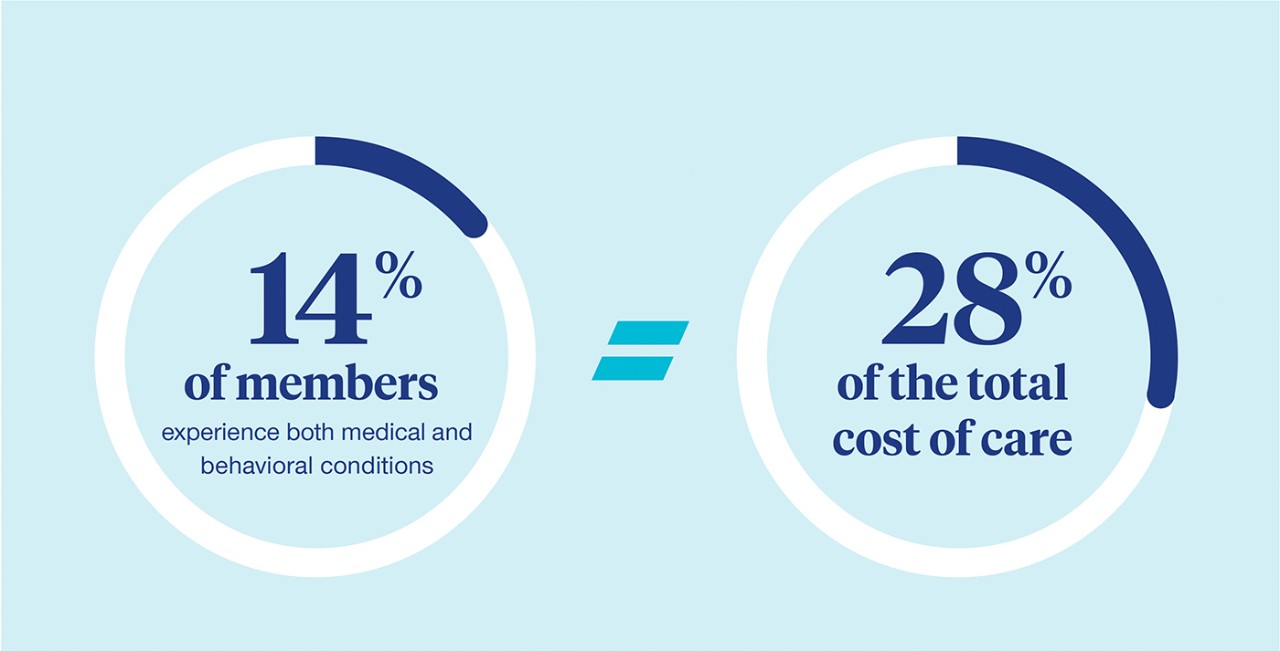
People with a mental health condition also experience higher morbidity and mortality rates compared to those without—mostly from untreated and preventable chronic physical conditions, such as cardiovascular disease, hypertension and diabetes.15
“Usually, when a behavioral health condition goes untreated, we’re likely to see higher levels of medical care such as inpatient stays and emergency room utilization,” says Stacie Grassmuck, director of behavioral health product and innovation for UnitedHealthcare Employer & Individual.
Integrated medical and behavioral benefits can address the full spectrum of health and well-being to provide whole-person care. When employers integrate behavioral, medical and pharmacy benefits, there is a single point of contact for an employee with a mental health condition who also has a chronic health condition.
“The integration of these benefits creates a more seamless experience with a single carrier. You also have better coordination between the benefits. For example, deciding whether to use an EAP benefit for mental health support or tapping into integrated benefits right away,” Randall says.
Planning for future behavioral health needs
History has shown that the mental health impact of disasters outlasts the physical impact, suggesting today’s elevated mental health need will continue despite the pandemic being deemed over.4 Employees with more severe behavioral health needs drive a disproportionate amount of an employer’s overall health spend. Of the top 10% insured that drive the highest costs, 27% had behavioral health care needs and accounted for 57% of health care costs.16
The challenges in the behavioral health landscape call on all stakeholders — including private and public insurers, care providers, employers and government policymakers — to innovate to better serve the behavioral health needs of everyone. Insurers can leverage data to forge new relationships with members, allowing for preventive interventions to address behavioral health needs.15
The challenges in the behavioral health landscape call on all stakeholders—including private and public insurers, care providers, employers and government policymakers—to innovate to better serve the behavioral health needs of everyone. Insurers can leverage data to forge new relationships with members, allowing for preventive interventions to address behavioral health needs.17
Through data-driven solutions, UnitedHealthcare works with employers to help identify gaps in care. For example, behavioral health claims utilization based on location, age, gender and other measures helps an employer understand if their employees may need mental health support to prevent a higher, more costly level of care.
“When behavioral health claims are lower than expected norms, it’s an indication that certain populations may not be getting the behavioral health support that they need,” says Craig Kurtzweil, chief analytics officer for UnitedHealthcare Employer & Individual. “We want to see employee utilization and strategies such as using an in-network or local provider, inpatient versus outpatient services and virtual care to help keep the costs lower for the employer.”
Employers are offering more differentiated behavioral health support that may help improve performance and retention.16 They’re also taking into account how they may contribute to overall well-being—recently citing mental and emotional health as the top well-being issue affecting their business followed by burnout, culture, virtual and hybrid work support and financial risk and stress.18
“Behavioral health treatment is effective. The response rate to therapy and medication is similar to a medical condition like diabetes,” Rosenzweig says. “We want to intervene early to help employees manage their everyday stress while offering solutions that support a range of mental health needs.”